News
Amy Kerdok '06 (Ph.D.) develops new instrumentation, advanced visualization schemes, and robotic platforms that support and advance robotic surgery.
Biomedical engineer Amy Kerdok (Ph.D. ’06) knows first hand how much a technological solution can affect a person’s life.
During her time on campus, Kerdok served as both “poobah” and women’s captain of the Harvard University Cycling Association. A well-rounded athlete, she led the team to success, but due to a congenital hiatial hernia, she suffered from gastroesophageal reflux disease (GERD) and frequently was ill while riding. (“My teammates just got used to it,”she says.)
Now a Clinical Development Engineer at Intuitive Surgical inSunnyvale, California, Kerdok develops new instrumentation, advanced visualization schemes, and robotic platforms that support and advance robotic surgery. In fact, Kerdok trusts in her company’s work so much that she actually arranged in 2009 to have an esophageal surgery performed on herself using the da Vinci robot that she develops at work.
Completely cured of GERD, she continues to cycle, is currently training to run the Boston marathon, and looks ahead with the hope of one day teaching engineering design to undergraduates.
What inspired you to pursue a career in biomedical engineering?
I have always been fascinated by how things work. As an athlete, I approached the human body as a machine, and I was intrigued by the physics of sport. Athletic themes have surrounded my life and my studies whether I was redesigning snowboard bindings, racing bicycles, or studying the energetics of running.
When I was 8 years old, I broke my ankle skiing. The doctors told me I might never walk the same again, and I had major reconstructive surgery. I was an active and curious kid, so the whole experience from the surgery to the physical therapy totally enthralled me. I realized I was going to be made whole again from these people—and their techniques and tools—and that was enough to make me want to learn to become one of them.
What was it about Harvard that made you want to earn your Ph.D. here?
I applied to the Harvard-MIT Health Sciences and Technology program because I wanted to deepen my understanding of both clinical and engineering basics. I actually began on the MIT side; however, as a Whitaker Fellow, I had the freedom of choosing whatever lab I wanted. After 18 lab visits, two of my top three were at Harvard. That was my first clue.
I decided to work with the late Prof. Tom McMahon, and while doing so quickly learned about all Harvard to offer and how it meshed more with my academic goals. I liked that I got to create my own plan of study, the interdisciplinary faculty, and the lack of mainstream departments. Combined, these aspects created a very fluid and family-oriented environment. Harvard felt individualized versus institutionalized, and that was a good fit for me.
What did you write your thesis on?
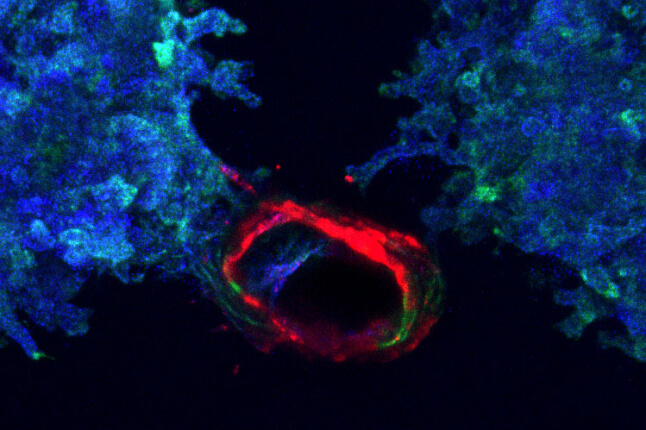
My master’s was on sports biomechanics, studying the energetics and mechanics of running on compliant surfaces. I wrote my Ph.D. thesis from Prof. Robert Howe’s lab on characterizing the nonlinear mechanical response of solid organs (the liver in particular) to surgical manipulation. The overall goal was to accurately characterize biological tissue under surgical stresses for the purposes of creating realistic surgical simulators.
What memory stands out the most from your time here?
There are two. The first was my time spent as a medical student doing a three-month internal medicine rotation at Mt. Auburn Hospital. The act of truly taking care of people—taking the time to learn their story and hear their struggles—was one of the most humbling and humanizing experiences of my life.
The other was teaching. Another grad student and I helped Prof. Howe revamp Engineering Sciences 51, “Computer-Aided Machine Design.” Teaching undergrads the art and excitement of engineering design from Tootsie Roll catapults to remote-control all-terrain vehicles (projects which I was thrilled to learn still exist today), rekindled my love for engineering design and aroused a desire to return to teaching someday.
What’s a typical day like in your current job?
There is no typical day—that is why I love my job.
It is my responsibility to investigate how surgeons use the da Vinci and decipher their needs into engineering specifications. So I get to travel the U.S. and the world to observe people using the da Vinci in various surgical situations. I take what I see back to the home office’s engineering and marketing teams, where I help write the clinical requirements of our various products, platforms, and software, and compose and run validations in a lab to prove their safety and effectiveness before launch. I also get to help with training—so there is some teaching involved.
I love the diversity of my job: part clinical, part technical, part marketing, and part business.
You’ve actually had a surgery performed on yourself, using the robotic device that you test at work. What was that like?
My procedure was elective: a Nissen fundoplication to correct a lifetime of GERD (gastroesophageal reflux disease). This is a procedure that can safely and effectively be done laparoscopically (straight sticks), but I had spent enough time in an O.R., and believed in our product so completely, that I wanted to get it done robotically. I knew I would get a better repair and would potentially have less pain and a faster recovery.
It was very different being on the O.R. table versus watching it from across the room. I recall that the last thing I did before "going under" was to check that the electrocautery settings were within the recommended range for use with our instrumentation. I also recorded data from my case, and it was really strange to later watch the video of my own surgery.
I am proud to say that all the hype about the da Vinci is true: I was on my feet again in no time and the result has dramatically improved the quality of my everyday life. And now I can really promote the da Vinci from both a patient and a technical perspective.
When designing instrumentation I always ask the engineers, “Would you put this in your mother?” After my surgery that question shifted to, “Would you use this on yourself?”
Has gender ever been an issue for you, as a female engineer?
I feel very comfortable as a female engineer. Yes, my undergraduate school was 20 percent women when I entered in 1993, but that never really bothered or hindered me. I was always a tomboy, and I liked working with men. Oddly, right now I work with three other women in our team of five clinical development engineers. Thus, on a day-to-day level there really are no issues.
However, there is still a definite gender gap and a glass ceiling in terms of female managers and the overall differences in pay scales between male and female engineers. Although this is frustrating, it is slowly changing, and I am confident that with time there will be more of a balance.
Where do you see yourself going from here, in your career? Can you see yourself moving back toward academia?
When I was finishing up my dissertation, I found I was torn. It was always my goal to go into industry, but I had this newfound love of teaching. Prof. Howe advised me that an “academic teaching engineering design is like a priest telling you how to be married.” He suggested I go out and get design/industry experience and then return to teach from experience.
As long as I’m learning and interested I will likely keep doing what I’m doing until the next opportunity/challenge comes along. Ultimately, the goal would be to return to academia to teach. I like the idea of introducing physics and engineering to students who otherwise may not consider those areas, and showing them that the problem solving skills learned in these disciplines can be applied in nearly any field.
Topics: Robotics, Health / Medicine, Bioengineering
Cutting-edge science delivered direct to your inbox.
Join the Harvard SEAS mailing list.