News
The first-in-human clinical phase I trial assessing the feasibility and safety of WDVAX, an immunostimulatory biomaterial-based cancer vaccine, in a cohort of 21 patients with stage 4 metastatic melanoma, was concluded with positive outcomes that encourage future vaccine developments and trials to test them in combination with immune checkpoint inhibitor therapies.
Mary Gooding, a patient who was treated with a cancer vaccine against her melanoma, in conversation with David Mooney in the Wyss Institute lab. Credit: Aram Boghosian for the Boston Globe.
The novel vaccine concept originated in the laboratory of David Mooney, the Robert P. Pinkas Family Professor of Bioengineering at SEAS. Together with his group at the Wyss Institute, Mooney and colleagues advanced the novel immunotherapy solution through a series of foundational studies. In addition to developing the capabilities needed to fabricate the biomaterial vaccines, Mooney’s group, in collaboration with that of Dr. Glenn Dranoff, who at the time was a Wyss Associate Faculty member and co-leader of Dana Farber Cancer Institute’s Cancer Vaccine Center, had carried out extensive preclinical studies to demonstrate the approach’s efficacy.
The trial was initiated in 2013 by the Wyss Institute at Harvard University and the Dana-Farber Cancer Institute and led by Dr. F. Stephen Hodi, Jr., director of DFCI’s Melanoma Center and Professor of Medicine at Harvard Medical School. The trial demonstrated that a precisely engineered biomaterial-based multi-component system is feasible to be consistently fabricated and applied to patients. The significant immune-activating functions of the monotherapy correlated with 43% of the patients exhibiting stable disease.
The team demonstrated that the vaccines can induce the regression of multiple types of tumors in animal models and, in addition, provided prophylactic protection. These foundational and translational efforts led up to the first-in-human WDVAX clinical trial assessing this new type of cancer vaccines whose results were recently published in Cancer Immunology Research.
The vaccination concept holds that a porous biomaterial scaffold made from a widely used biodegradable medical polymer and infused with bioactive molecules can function as a training ground for the immune system. By infusing the scaffold with the cytokine molecule GM-CSF, dendritic cells – central orchestrators of immune responses – are recruited into the porous scaffold interior, where they are activated by additionally infused CpG oligonucleotides that function as an adjuvant.
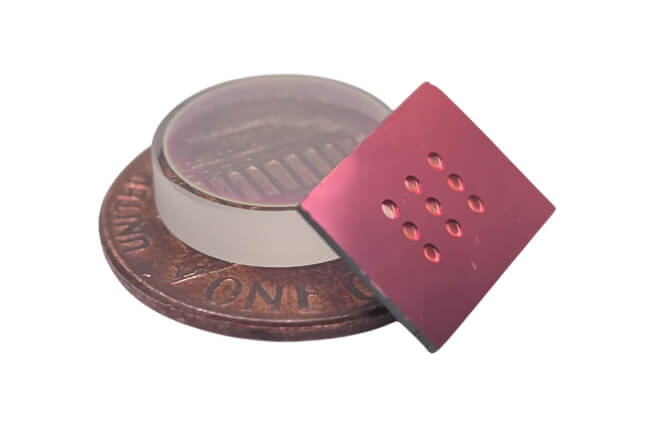
The personalized biomaterial-based cancer vaccine consists of a porous biomaterial scaffold the size of an aspirin tablet that is infused with immune cell-recruiting and activating molecules and inactivated tumor antigens derived from tumors of the trial participants. Credit: Wyss Institute at Harvard University
To prime dendritic cells specifically against cancer cells, the WDVAX trial team loaded the scaffold with inactivated tumor antigens derived from tumors of the trial participants. The Mooney and Dranoff team’s preclinical studies had shown that, upon their activation, the reprogrammed DCs migrate from the scaffold to nearby lymph nodes where they activate T cells that engage in a coordinated attack on tumor cells.
The development and study of the personalized cancer vaccine was funded by the Wyss Institute, DFCI, and the National Institutes of Health, and the crucial technologies invented for their realization are owned or co-owned by Harvard, DFCI, and the University of Michigan.
From feasibility to immune activation
To demonstrate the clinical feasibility of WDVAX therapy in a dose-escalation study of melanoma patients, the trial’s goal was to show that a fabrication process could be put into place that was able to produce sufficient WDVAX vaccines within 28 days following the resection of patients’ tumors to allow for multiple consecutive treatments of the same patients with personalized vaccines.
Using the Mooney lab’s proprietary recipe, team members at DFCI’s Cell Manipulation Core Facility loaded inactivated tumor antigens contained in lysed tumor samples into the biomaterial scaffolds and successfully manufactured WDVAX vaccines in a beneficial time frame for all patients of the 15-patient expansion cohort. They also succeeded in producing sufficient vaccine for seven out of eight additional trial participants. The study thus established a clinically applicable vaccine manufacturing process and showed that vaccine fabrication per se likely won’t be a bottleneck for evaluating similar types of biomaterials-based vaccines in future trials.
To introduce WDVAX vaccines into patients’ bodies, surgeons on the team simply had to make a small incision in the upper arm or thighs, implant the manufactured vaccines under the skin, and suture the wound. The patients were then closely monitored for signs of immune reactions and often exhibited a significant local response at the implant site.
Next to evaluate the feasibility of conducting WDVAX clinical trials, the team’s other goals were to assess the overall survival of the vaccine recipients and to analyze their immune responses. After receiving their tumor-specific WDVAX vaccines, none of the patients developed treatment-related adverse events with life-threatening consequences and, importantly, 43% of all patients in the entire cohort had stable disease.
Upon closer comparative examination of patients’ tumor microenvironments by comparing tissue samples prior and following vaccination, the researchers found that T cells and other types of immune cells were indeed induced. Specifically, the numbers of CD4+ T cells that normally coordinate immune attacks within tumors were found to be variably increased by WDVAX vaccines, and the researchers observed heterogeneous infiltration of tumors by cytotoxic CD8+ T cells with tumor cell-killing potential as well as of myeloid cells of the immune system.
At the same time, they also found that T cells that entered tumors upon WDVAX vaccination, upregulated so-called checkpoint proteins. Checkpoint proteins generally act as “brakes” that prevent T cells from attacking tumor cells. Hodi, Mooney, and the team therefore speculate that taking a two-pronged approach in future clinical trials could be promising. By combining WDVAX-like vaccines with widely used checkpoint inhibitor therapy, a tumor-specific T cell response could be launched in tumor environments in which the immune system’s ability to fight the tumors would be additionally enhanced. Such a coordinated immunotherapy could advance treatment success to potentially enable the regression of tumors, as seen by Mooney’s group for monotherapy with WDVAX vaccines alone in preclinical animal models carrying aggressive melanoma tumors.
“Since the WDVAX trial was started, our and other groups have made a number of important advances in the biomaterial cancer vaccine space. Next-generation injectable [not implantable] scaffolds have emerged that among other favorable characteristics have the ability to further shape immune responses. Also, the technological capabilities of identifying patient-specific tumor antigens with immune-activating potential are constantly evolving,” said Mooney. “We are confident that integrating these newer insights in next-generation approaches and combining those with other forms of immunotherapy, including checkpoint inhibitor therapy can result in new breakthroughs in the treatment of patients suffering from different types of cancer.”
Topics: Bioengineering, Health / Medicine, Research
Cutting-edge science delivered direct to your inbox.
Join the Harvard SEAS mailing list.
Scientist Profiles
David Mooney
Robert P. Pinkas Family Professor of Bioengineering
Press Contact
Anne J. Manning | amanning@seas.harvard.edu