News
A patient receives care following a knee replacement surgery. A new vaccine strategy could protect such patients from infections.
Patients with implanted medical devices like orthopedic joint replacements, pacemakers, and artificial heart valves run a small but significant risk that these devices get infected with bacterial pathogens. This starts them on a burdensome path requiring “redo” (revision) surgeries, prolonged antibiotic treatments, or in severe cases amputation. If the infections spread in patients’ bodies, they can even become fatal.
Researchers have long pursued the idea that vaccines could protect patients against the pathogen Staphylococcus aureus, the leading cause of orthopedic device infection. But so far, an effective vaccine has not been produced despite much effort and several large pharma-led clinical trials.
Now, clinical researchers and bioengineers at the Harvard John A. Paulson School of Engineering and Applied Sciences (SEAS) and the Wyss Institute for Biologically Inspired Engineering have developed a novel vaccine strategy with the potential to solve the challenge of device infection in patients. Their approach uses slowly biodegradable, injectable biomaterial scaffold vaccines that are equipped with immune cell attracting and stimulating molecules and S. aureus-specific antigens.
Applied to a mouse model of orthopedic device infection, the vaccines created a beneficial immune response that decreased the bacterial burden about 100-fold more effectively than much shorter-lived conventional control vaccines. Biomaterial vaccines made with antigens from antibiotic-sensitive S. aureus (MSSA) bacteria also protected devices against infection from antibiotic-resistant S. aureus (MRSA) strains, making future off-the-shelf vaccines for broad use in orthopedic surgeries an attractive possibility. The findings are published in Proceedings of the National Academy of Sciences.
The study was led by David Mooney, the Robert P. Pinkas Family Professor of Bioengineering at SEAS and a founding core faculty member at the Wyss Institute. Mooney previously pioneered biomaterials-based vaccines as novel immunotherapies in the fight against cancer and, more recently, to help prevent sepsis and septic shock in small and large animal models. Mooney’s team showed that these types of vaccines can activate the immune system with high efficiency against tumor cells and pathogens.
“In this study, we are seeing the type of immune responses involving specific T cell populations that might have been missing in patients vaccinated with conventional vaccines in clinical trials, in addition to S. aureus-specific antibody responses that are also produced by soluble vaccine formulations,” Mooney said. “In combination with optimized antigen collections derived from S. aureus species, our approach could lead to novel biomaterials-based vaccines with the potential to save lives and improve health outcomes for patients globally.”
In the U.S. alone, about 790,000 total knee replacements and more than 450,000 hip replacements are currently performed by orthopedic surgeons; up to 2-4% of those implanted devices will become infected, noted Alexander Tatara, assistant professor at The University of Texas Southwestern Medical Center in Dallas and first author of the study. “These numbers alone highlight the urgency of finding effective countermeasures and bringing them to patients fast,” Tatara said.
Protection powered by PAMPs
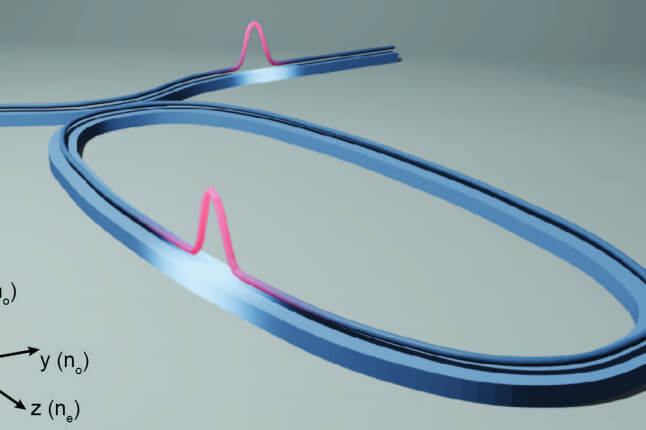
The biomaterial vaccines, upon their injection, provide a molecular training ground for dendritic cells — central coordinators of the immune system that orchestrate a complex T cell response against the pathogen in nearby lymph nodes.
"To specifically program [dendritic cells] against infectious S. aureus bacteria, we incorporated immunogenic antigen components derived from disrupted bacteria into our vaccines, which we captured using the Wyss Institute’s FcMBL technology,” said co-author Michael Super, who developed the technology with Wyss founding director Donald Ingber. FcMBL is an engineered immune protein capable of binding to more than 200 different pathogens and their glycosylated surface-exposed molecules commonly known as “pathogen-associated molecular patterns,” in short PAMPs. “In this vaccine we incorporate a diverse repertoire of hundreds of FcMBL-bound S. aureus PAMP antigens, instead of only one or few antigens contained in conventional vaccines, and enable efficient antigen transfer to DCs following injection of our vaccines into mice,” said Super, who is the Wyss Institute’s Director of Immuno-Materials.
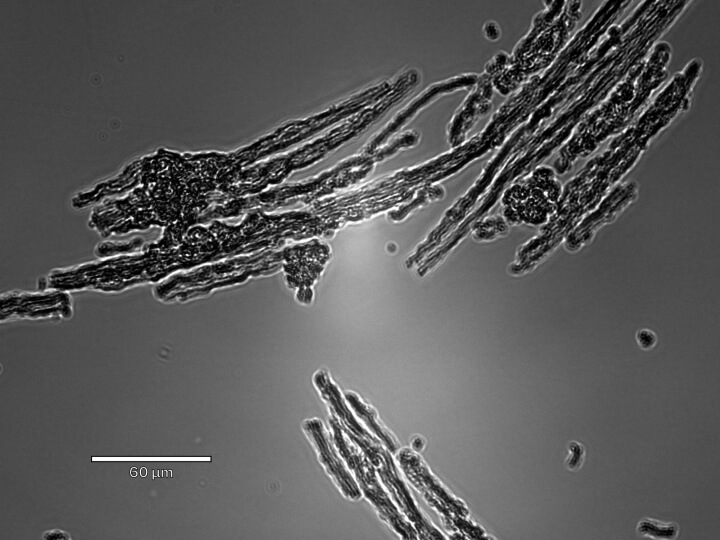
S. aureus colonies.
In mice that the researchers vaccinated with their biomaterial vaccine and challenged with pathogenic S. aureus bacteria, this strategy reduced the overall bacterial burden much more potently than soluble control vaccines containing the same molecular components.
“Likely by being able to engage the immune system in a sustained and highly concerted way, our biomaterial vaccines are able to activate distinct types of so-called T helper cells that start to secrete a number of protective cytokine molecules. Conventional soluble vaccines, whose molecular components quickly diffuse in the tissue they are injected in, were less efficient at this,” said Tatara, who spearheaded the project when he was a clinical research fellow in Mooney’s group at Harvard. “We will have to figure out in much more depth which parts of the immune system exactly are responsible and cooperate to bring about the protective effects.”
Proof of vaccination
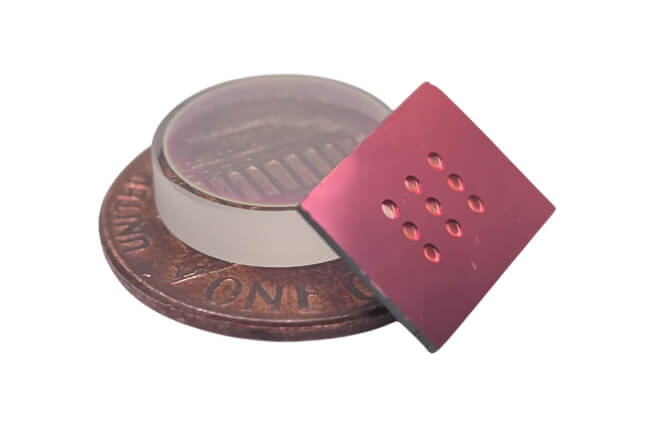
The team translated their observations into a mouse model of actual orthopedic device infection in which a small device is implanted into one of the animals’ hind legs and infected with a dose of pathogenic S. aureus bacteria. Five weeks prior to the surgery, they started the animals on a vaccination protocol using biomaterial and soluble control vaccines. When the researchers quantified the bacteria that managed to grow on the implanted devices, they found that their biomaterial strategy suppressed bacterial growth about 100-fold stronger than the soluble vaccine formulation.
“Importantly, we found that a biomaterial vaccine we fabricated with antigens from ‘methicillin-sensitive S. aureus’ (MSSA) strains can also protect implanted devices against later infection from methicillin-resistant (MRSA) strains, which are a big problem in hospital settings,” said Tatara. “Also trying to tease out which PAMPs stimulate the immune system the strongest opens a new avenue of research that could lead to more minimal, yet highly effective vaccines.”
Mooney’s team showed that this approach could indeed be rewarding. By analyzing PAMPs from a S. aureus strain, identifying a PAMP signature, and then using one of the PAMPs as a single antigen in a biomaterial vaccine, they already could provide some level of device protection in mice. “One could envision a future in which clinical researchers rapidly identify relevant PAMPs in patient-specific S. aureus strains obtained through simple non-invasive procedures ahead of surgeries to produce effective personalized biomaterial vaccines that protect implanted orthopedic devices from infections,” said Tatara.
The study was also authored by Shanda Lightbown, Shawn Kang, Wei-Hung Jung, Hamza Ijaz, Jean Lee, and Sandra Nelson. It was supported by awards from the National Institutes of Health (award# T32 AI007061 and NIH K08 AI180362), Harvard Catalyst (award# UM1TR004408), as well as financial contributions from the Wyss Institute, and Harvard with its affiliated academic healthcare centers.
Topics: Bioengineering, Health / Medicine, Research, Technology
Cutting-edge science delivered direct to your inbox.
Join the Harvard SEAS mailing list.
Scientist Profiles
David Mooney
Robert P. Pinkas Family Professor of Bioengineering
Press Contact
Anne J. Manning | amanning@seas.harvard.edu